2020-10-21 14:26:49
Prelude
Today’s Topics
- The neuroscience of psychiatric disorders
- Major affective (mood) disorders
- Major Depressive Disorder (depression)
- Bipolar Disorder
Mental illness lifetime prevalence
Neuroscience of psychiatric disorders
- Diseases of the mind as disorders of the brain
- System-wide effects; no single or simple cause
- Heritability
- proportion of variance in trait accounted for by genetic factors
- Higher for psychiatric disorders than non-psychiatric diseases
- Family member with mental illness highest known risk factor
Depression
Major Depressive Disorder
- Symptoms
- Unhappy mood, insomnia, lethargy, loss of pleasure, interest, energy
- Agitation
- Lasting for several weeks or more
Depression
- Experienced by ~7% Americans in any year
- Prevalence (up to ~20% lifetime)
- Females 2-3x males, higher 40+ years of age
- Heritability (large, 2.5 M Swedish population study)
- Females 0.49 (twins); 0.51 (non-twin relatives)
- Males 0.41 (twins); 0.36 (non-twin relatives)
- (Kendler, Ohlsson, Lichtenstein, Sundquist, & Sundquist, 2018)
Symptoms, (Mahar, Bambico, Mechawar, & Nobrega, 2014)
Neurobiology of Major Depressive Disorder (MDD)
- Reduced sizes of brain regions
- Hypoactivity
- Pharmacological factors
- Synaptic dysfunction
Neurological factors
- Reduced hippocampal volumes
- (Videbech & Ravnkilde, 2004a) meta-analysis
(Videbech & Ravnkilde, 2004a)
Left Hippocampus
(Videbech & Ravnkilde, 2004b)
Right Hippocampus
Neurological factors
- Hypoactivity in
- Frontal and temporal cortex
- Anterior cingulate
- Insula
- Cerebellum
- (Fitzgerald, Laird, Maller, & Daskalakis, 2008)
(Fitzgerald et al., 2008)
- patients v. controls, (b) patients on SSRIs, (c) patients v. ctrls (happy stim), (d) patients v. controls (sad stim)
Baseline hyperactivity (Hamilton et al., 2012)
Valence-specific hyperactivity (Hamilton et al., 2012)
Disrupted connectivity
- Resting state fMRI (rsFMRI) in \(n=421\) patients with major depressive disorder and \(n=488\) control subjects.
- Reduced connectivity between orbitofrontal cortex (OFC) and other areas of the brain
- Increased connectivity between lateral PFC and other brain areas
Pharmacological factors
- Endocrine
- Thyroid dysfunction (Medici et al., 2014)
- Altered cortisol reactivity (Burke, Davis, Otte, & Mohr, 2005)
Pharmacological factors
- Monoamine hypothesis
- More: euphoria
- Less: depression
- Resperine (antagonist for NE & 5-HT) can cause depression
- Low serotonin (5-HT) metabolite levels in CSF of suicidal depressives (Samuelsson, Jokinen, Nordström, & Nordström, 2006)
Measuring 5-HT
- CSF, platelets, plasma, urine, saliva
- CSF & platelets correlate highly (Audhya, Adams, & Johansen, 2012)
- Salivary 5-HT does not correlate with mood symptoms (Leung et al., 2018)
Treatments for depression
- Psychotherapy
- Often effective when combined with drug treatment
- Exercise
- Drugs
Drugs
- Monoamine oxidase (MAO) inhibitors
- MAO destroys excess monoamines in terminal buttons
- MAO-I’s boost monoamine levels
- Tricyclics
- Inhibit NE, 5-HT reuptake
- Upregulate monoamine levels, but non-selective = side effects
Drugs
- Selective Serotonin Reuptake Inhibitors (SSRIs)
- Fluoxetine (Prozac, Paxil, Zoloft)
- Prolong duration of 5-HT in synaptic cleft
- Also increase brain steroid production
- Selective Serotonin Norepinephrine Reuptake Inhibitors (SNRIs)
Cymbalta (SNRI)
How well do the drugs work?
- STAR*D trial
- On SSRI for 12-14 weeks. ~1/3 achieved remission; 10-15% showed symptom reduction.
- If SSRI didn’t work, could switch drugs. ~25% became symptom free.
- 16% of participants dropped out due to tolerability issues
- Took 6-7 weeks to show response.
Who will benefit from drug therapy?
- Depends on
- Early life stress
- Brain (amygdala) response to emotional faces
- (Goldstein-Piekarski et al., 2016)
- Low-stress + low amyg reactivity -> > responding
- High stress + high amyg reactivity -> > responding
Monoamine hypothesis of depression
- Disrupted (lowered) levels of monoamines (especially NE & 5-HT) result in depression
Problems with monoamine hypothesis
- Too simplistic
- NE, 5-HT interact
- Drugs fast acting (min), but improvement slow (weeks)
“No correlation between serotonin and its metabolite 5-HIAA in the cerebrospinal fluid and [11C]AZ10419369 binding measured with PET in healthy volunteers.” (Tiger et al., 2015)
“…we performed the first meta-analysis of the mood effects in [acute tryptophan depletion] ATD and [alpha-methyl-para-tyrosine] APTD studies. The depletion of monoamine systems (both 5-HT and NE/DA) does not decrease mood in healthy controls. However, in healthy controls with a family history of MDD the results suggest that mood is slightly decreased…by [monoamine depletion]…”
What do drugs do, then?
- Alter receptor sensitivity?
- Serotonin presynaptic autoreceptors compensate
- Postsynaptic upregulation of NE/5-HT effects
What do drugs do, then?
- Stimulate neurogenesis?
- Link to neurotrophin, brain-derived nerve growth factor (BDNF)
- BDNF boosts neurogenesis
- SSRIs stimulate growth of new neurons in hippocampus
Neurogenesis hypothesis, (Mahar et al., 2014)
- Chronic stress causes neural loss in hipp
- Chronic stress downregulates 5-HT sensitivity
- Depression ~ chronic stress
- Anti-depressants upregulate neurogenesis via 5-HT modulation
Ketamine
- Selective antagonist of the NMDA receptor, an ionotropic glutamate receptor
- Relieves depressive symptoms relatively quickly (Berman et al., 2000) and (Zarate et al., 2006)
- Boosts synaptic spine formation (Li et al., 2010) and reverses effects of induced stress
Electroconvulsive Therapy (ECT)
- Last line of treatment for drug-resistant depression
- Electric current delivered to the brain causes 30-60s seizure.
- ECT usually done in a hospital’s operating or recovery room under general anesthesia.
- Once every 2 - 5 days for a total of 6 - 12 sessions.
Electroconvulsive Therapy (ECT)
- Remission rates of up to 50.9% (Dierckx, Heijnen, Broek, & Birkenhäger, 2012)
- Seems to work via
- Anticonvulsant (block Na+ channel or enhance GABA function) effects
- Neurotrophic (stimulates neurogenesis) effects
Patients speak
- Kitty Dukakis’ (wife of former Governor/Presidential candidate Michael Dukakis) story: http://www.nytimes.com/2016/12/31/us/kitty-dukakis-electroshock-therapy-evangelist.html
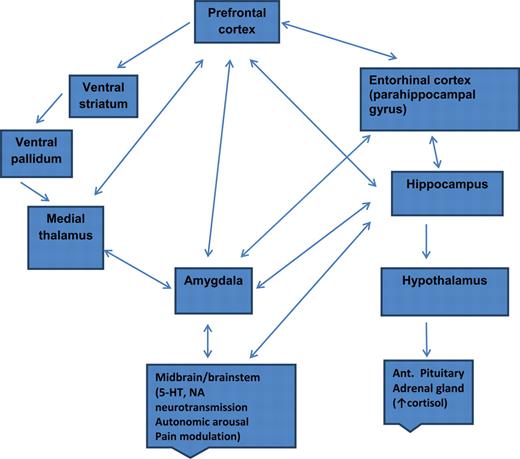
Depression’s widespread impact
- Widespread brain dysfunction
- Prefrontal cortex, amygdala, HPA axis, circadian rhythms
- Genetic + environmental factors
- Disturbance in 5-HT, NE systems, cortisol
- Many sufferers do not respond to available treatments
Points on depression
- Drug treatments affect neuromodulator NT systems, but
- Can’t effectively measure NT levels
- Neuromodulators interact, so many side-effects
- ‘Monoamine hypothesis’ of depression is at-best incomplete
- ‘Talk’ therapies can change behavior/mood by creating new/strengthened circuits
Bipolar disorder
Bipolar disorder
- Formerly “manic depression” or “manic depressive disorder”
- Alternating mood states
- Mania or hypomania (milder form)
- Depression
- Cycles 3-6 mos in length, but
- Rapid cycling (weeks or days)
- Suicide risk 20-60x normal population, (Baldessarini, Pompili, & Tondo, 2006)
Symptoms
Prevalence, subtypes
- 1-3% prevalence, subthreshold affects another 2%
- Subtypes
- Bipolar I: manic episodes, possible depressive ones
- Bipolar II: no manic episodes but hypomania (disinhibition, irritability/agitation) + depression
Related symptoms
- Psychosis (hallucinations or delusions)
- Anxiety, attention-deficit hyperactivity disorder (ADHD)
- Substance abuse
Genetics
- Overlap between bipolar disorder and schizophrenia
- Genes for voltage-gated Ca++ channels
- Regulate NT, hormone release
- Gene expression, cell metabolism
- (Craddock & Sklar, 2013)
Brain responses to emotional faces ≠ depression
(Lawrence et al., 2004)
(Lawrence et al., 2004)
Amyg, Hip volume reduced; ventricles larger
(Hallahan et al., 2011)
Drug treatments
- Mood stabilizers
- Lithium (Li)
- Valproate (Depakote)
- Anticonvulsants
- GABA agonists
- Usually to treat epilepsy
- e.g. lamotrigine (Lamictal)
- Atypical antipsychotics
Lithium “discovered” accidentally
- Injections of manic patients’ urine with lithium compound (chemical stabilizer) into guinea pig test animals
- Had calming effect
- John Cade discovered in 1948
- Earliest effective medications for treating mental illness
Effects of Lithium
- Reduces mania, minimal effects on depressive states
- Preserves PFC, hip, amyg volume
- downregulates DA, glu; upregulates GABA
- modulates 5-HT, NE
- levels can be tested/monitored via blood test
- (Malhi, Tanious, Das, Coulston, & Berk, 2013)
Other treatment options
- Psychotherapy
- Electroconvulsive Therapy (ECT)
- Sleep medications
Prospects
- STEP-BD cohort (n=1469)
- 58% achieved recovery
- 49% had recurrences within 2 years
- Residual depressive symptoms can persist
- (Geddes & Miklowitz, 2013)
An Unquiet Mind
BP summed-up
- Changes in mood, but ≠ depression
- Genetic + environmental risk
- Changes in emotion processing network activity, size of hippocampus
- Heterogeneous
- No simple link to a specific NT system
Next time…
- Schizophrenia
References
Audhya, T., Adams, J. B., & Johansen, L. (2012). Correlation of serotonin levels in CSF, platelets, plasma, and urine. Biochimica et Biophysica Acta, 1820(10), 1496–1501. https://doi.org/10.1016/j.bbagen.2012.05.012
Baldessarini, R. J., Pompili, M., & Tondo, L. (2006). Suicide in Bipolar Disorder: Risks and Management. CNS Spectrums, 11(06), 465–471. https://doi.org/10.1017/S1092852900014681
Berman, R. M., Cappiello, A., Anand, A., Oren, D. A., Heninger, G. R., Charney, D. S., & Krystal, J. H. (2000). Antidepressant effects of ketamine in depressed patients. Biol. Psychiatry, 47(4), 351–354. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/10686270
Burke, H. M., Davis, M. C., Otte, C., & Mohr, D. C. (2005). Depression and cortisol responses to psychological stress: A meta-analysis. Psychoneuroendocrinology, 30(9), 846–856. https://doi.org/10.1016/j.psyneuen.2005.02.010
Cheng, W., Rolls, E. T., Qiu, J., Liu, W., Tang, Y., Huang, C.-C., … Feng, J. (2016). Medial reward and lateral non-reward orbitofrontal cortex circuits change in opposite directions in depression. Brain, aww255. https://doi.org/10.1093/brain/aww255
Craddock, N., & Sklar, P. (2013). Genetics of bipolar disorder. The Lancet, 381(9878), 1654–1662. https://doi.org/10.1016/S0140-6736(13)60855-7
Dierckx, B., Heijnen, W. T., Broek, W. W. van den, & Birkenhäger, T. K. (2012). Efficacy of electroconvulsive therapy in bipolar versus unipolar major depression: A meta-analysis. Bipolar Disorders, 14(2), 146–150. https://doi.org/10.1111/j.1399-5618.2012.00997.x
Fitzgerald, P. B., Laird, A. R., Maller, J., & Daskalakis, Z. J. (2008). A meta-analytic study of changes in brain activation in depression. Human Brain Mapping, 29(6), 683–695. https://doi.org/10.1002/hbm.20426
Geddes, J. R., & Miklowitz, D. J. (2013). Treatment of bipolar disorder. The Lancet, 381(9878), 1672–1682. https://doi.org/10.1016/S0140-6736(13)60857-0
Goldstein-Piekarski, A. N., Korgaonkar, M. S., Green, E., Suppes, T., Schatzberg, A. F., Hastie, T., … Williams, L. M. (2016). Human amygdala engagement moderated by early life stress exposure is a biobehavioral target for predicting recovery on antidepressants. Proceedings of the National Academy of Sciences, 113(42), 11955–11960. https://doi.org/10.1073/pnas.1606671113
Hallahan, B., Newell, J., Soares, J. C., Brambilla, P., Strakowski, S. M., Fleck, D. E., … McDonald, C. (2011). Structural Magnetic Resonance Imaging in Bipolar Disorder: An International Collaborative Mega-Analysis of Individual Adult Patient Data. Biological Psychiatry, 69(4), 326–335. https://doi.org/10.1016/j.biopsych.2010.08.029
Hamilton, J. P., Etkin, A., Furman, D. J., Lemus, M. G., Johnson, R. F., & Gotlib, I. H. (2012). Functional neuroimaging of major depressive disorder: A Meta-Analysis and new integration of baseline activation and neural response data. AJP, 169(7), 693–703. https://doi.org/10.1176/appi.ajp.2012.11071105
Kendler, K. S., Ohlsson, H., Lichtenstein, P., Sundquist, J., & Sundquist, K. (2018). The genetic epidemiology of treated major depression in sweden. The American Journal of Psychiatry, 175(11), 1137–1144. https://doi.org/10.1176/appi.ajp.2018.17111251
Lawrence, N. S., Williams, A. M., Surguladze, S., Giampietro, V., Brammer, M. J., Andrew, C., … Phillips, M. L. (2004). Subcortical and ventral prefrontal cortical neural responses to facial expressions distinguish patients with bipolar disorder and major depression. Biological Psychiatry, 55(6), 578–587. https://doi.org/10.1016/j.biopsych.2003.11.017
Leung, J., Selvage, C., Bosdet, T., Branov, J., Rosen-Heath, A., Bishop, C., … Horvath, G. (2018). Salivary serotonin does not correlate with central serotonin turnover in adult phenylketonuria (PKU) patients. Molecular Genetics and Metabolism Reports, 15, 100–105. https://doi.org/10.1016/j.ymgmr.2018.03.008
Li, N., Lee, B., Liu, R.-J., Banasr, M., Dwyer, J. M., Iwata, M., … Duman, R. S. (2010). mTOR-dependent synapse formation underlies the rapid antidepressant effects of NMDA antagonists. Science, 329(5994), 959–964. https://doi.org/10.1126/science.1190287
Mahar, I., Bambico, F. R., Mechawar, N., & Nobrega, J. N. (2014). Stress, serotonin, and hippocampal neurogenesis in relation to depression and antidepressant effects. Neuroscience & Biobehavioral Reviews, 38, 173–192. https://doi.org/10.1016/j.neubiorev.2013.11.009
Malhi, G. S., Tanious, M., Das, P., Coulston, C. M., & Berk, M. (2013). Potential Mechanisms of Action of Lithium in Bipolar Disorder. CNS Drugs, 27(2), 135–153. https://doi.org/10.1007/s40263-013-0039-0
Medici, M., Direk, N., Visser, W. E., Korevaar, T. I. M., Hofman, A., Visser, T. J., … Peeters, R. P. (2014). Thyroid function within the normal range and the risk of depression: A population-based cohort study. J. Clin. Endocrinol. Metab., 99(4), 1213–1219. https://doi.org/10.1210/jc.2013-3589
Palazidou, E. (2012). The neurobiology of depression. British Medical Bulletin, 101, 127–145. https://doi.org/10.1093/bmb/lds004
Ruhé, H. G., Mason, N. S., & Schene, A. H. (2007). Mood is indirectly related to serotonin, norepinephrine and dopamine levels in humans: A meta-analysis of monoamine depletion studies. Molecular Psychiatry, 12(4), 331–359. https://doi.org/10.1038/sj.mp.4001949
Samuelsson, M., Jokinen, J., Nordström, A.-L., & Nordström, P. (2006). CSF 5-HIAA, suicide intent and hopelessness in the prediction of early suicide in male high-risk suicide attempters. Acta Psychiatrica Scandinavica, 113(1), 44–47. https://doi.org/10.1111/j.1600-0447.2005.00639.x
Tiger, M., Svenningsson, P., Nord, M., Jabre, S., Halldin, C., & Lundberg, J. (2015). No correlation between serotonin and its metabolite 5-HIAA in the cerebrospinal fluid and [11C]AZ10419369 binding measured with PET in healthy volunteers. Retrieved from http://hdl.handle.net/10616/44513
Videbech, P., & Ravnkilde, B. (2004a). Hippocampal volume and depression: A meta-analysis of MRI studies. Am. J. Psychiatry, 161(11), 1957–1966. https://doi.org/10.1176/appi.ajp.161.11.1957
Videbech, P., & Ravnkilde, B. (2004b). Hippocampal volume and depression: A meta-analysis of mri studies. American Journal of Psychiatry, 161(11), 1957–1966. https://doi.org/10.1176/appi.ajp.161.11.1957
Zarate, C. A., Jr, Singh, J. B., Carlson, P. J., Brutsche, N. E., Ameli, R., Luckenbaugh, D. A., … Manji, H. K. (2006). A randomized trial of an N-methyl-D-aspartate antagonist in treatment-resistant major depression. Arch. Gen. Psychiatry, 63(8), 856–864. https://doi.org/10.1001/archpsyc.63.8.856