2020-11-10 09:36:02
Prelude
Prelude
Announcements
- Exam 3 next Tuesday, November 17
- Grading
- Best 3 of 4 quizzes
- Best 3 of 4 exams
- Blogs or paper
Today’s Topics
- Wrap-up on pain
- The neuroscience of action
Pain
Pain in the brain
Pain in the brain
“…we used machine-learning analyses to identify a pattern of fMRI activity across brain regions — a neurologic signature — that was associated with heat-induced pain. The pattern included the thalamus, the posterior and anterior insulae, the secondary somatosensory cortex, the anterior cingulate cortex, the periaqueductal gray matter, and other areas…”
Pain relief
- Prostaglandins
- hormone-like effects, but released in many places
- trigger vasodilation and inflammation
Pain relief
- Paracetymol (acetaminophen)
- Mechanism not fully understood
- inhibits synthesis of prostaglandins via cyclooxygenase (COX) enzyme
- may modulate endocannabinoid system
- Nonsteroidal anti-inflamatory drugs (NSAIDs): aspirin, ibuprofen
- Also inhibit prostaglandins via COX
Pain relief
- Opioids
- Activate endogenous opioid systems
- multiple receptor types (\(\delta\), \(\kappa\), \(\mu\),…)
- peripheral sensory neurons, amygdala, hypothalamus, PAG, spinal cord, cortex, medulla, pons,…
- brainstem opioid neurons provide descending inhibition of nociceptors


Pain relief
- Capsaicin
- Binds to TRPV1 receptor in thermo/nociceptors
- Alters how peripheral neuron responds to mechanical stimulation
- (Borbiro, Badheka, & Rohacs, 2015)
Pain relief
- Why rubbing can help
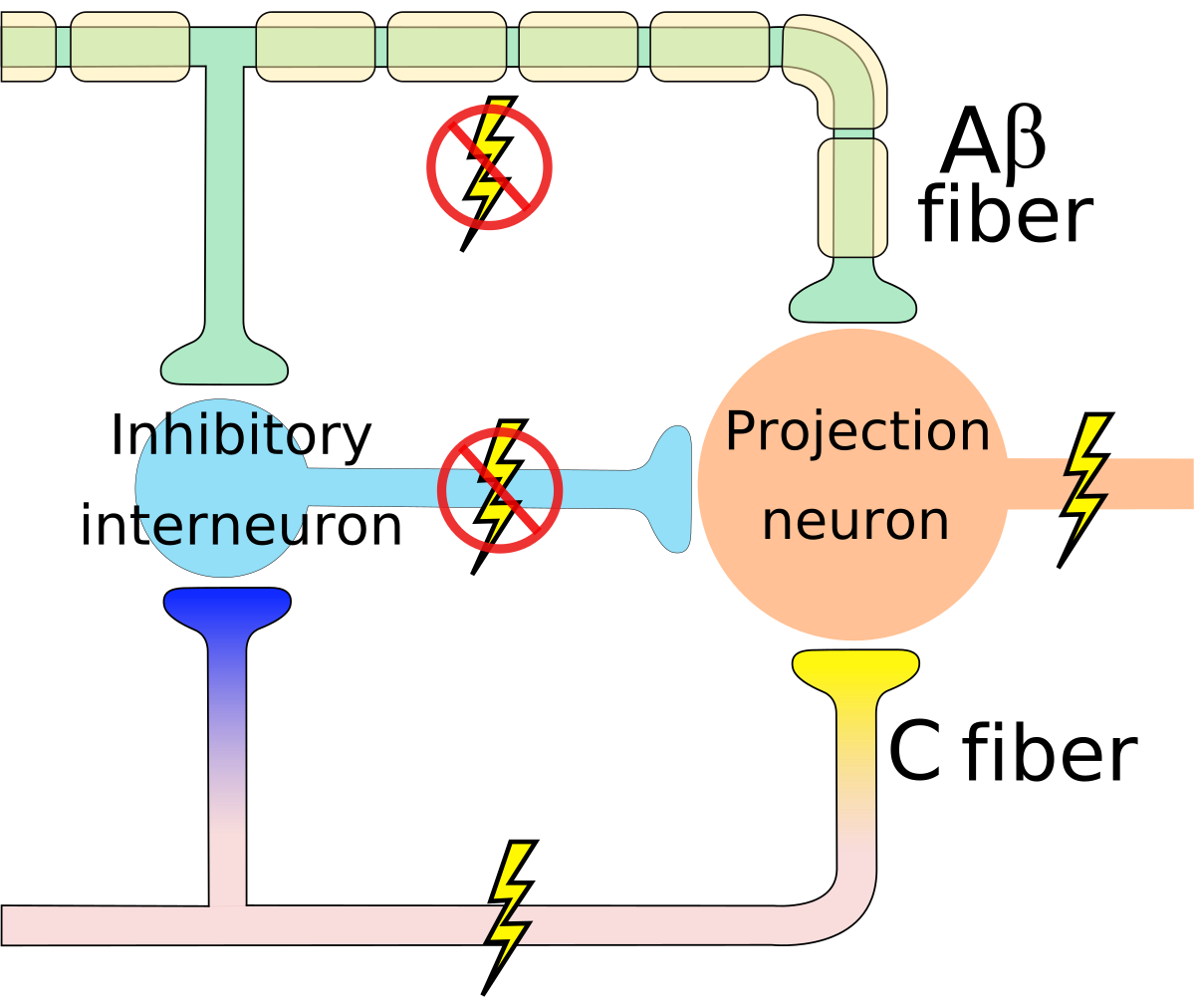
Gate control theory (Melzack & Wall, 1965)
Gate control theory (Melzack & Wall, 1965)
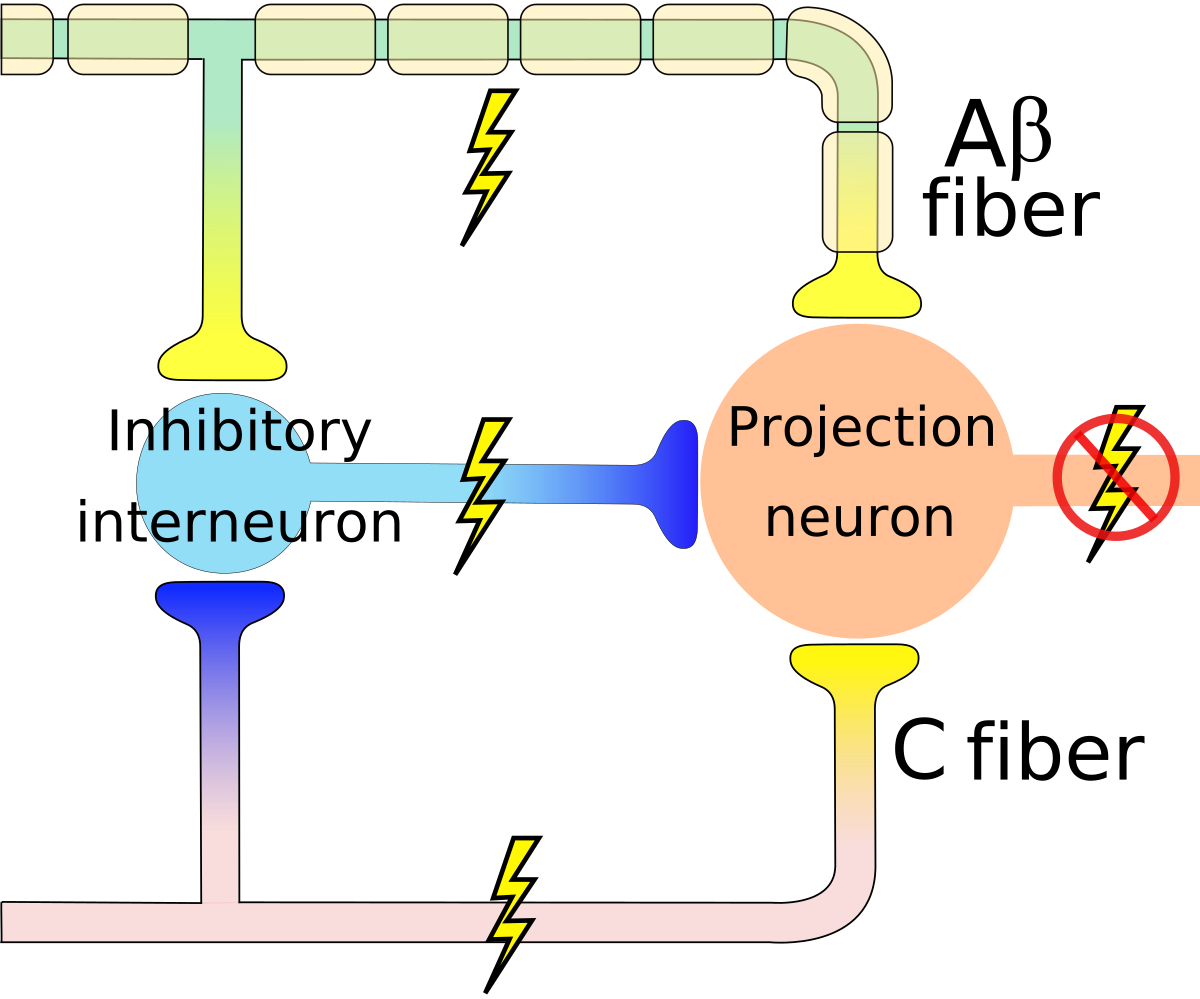
By self - self-made in Inkscape, CC BY-SA 3.0, Link
Psychological and physical dimensions

(Papini, Fuchs, & Torres, 2015)
Summary
- Pain
- Multiple receptor channels
- Highly interconnected CNS network
- Multiple targets for modulation
Action
The neuroscience of action
- What types of actions are there?
- How are they produced?
- By the muscles
- By the nervous system
Remember
- Nervous system “output” includes
- Movements
- Autonomic responses
- Endocrine responses
Types of actions
- Reflexes
- Simple, highly stereotyped, unlearned, rapid
- vs. Planned or voluntary actions
- Complex, flexible, acquired, slower
- Discrete (reaching) vs. rhythmic (walking)
- Ballistic (no feedback) vs. controlled (feedback)
Multiple, parallel controllers
Key “nodes” in network
- Primary motor cortex (M1)
- Non-primary motor cortex
- Basal ganglia
- Brain stem
- Cerebellum
- Spinal cord
Muscle classes
- Axial
- Trunk, neck, hips
- Proximal
- Shoulder/elbow, pelvis/knee
- Distal
- Hands/fingers, feet/toes
Muscles
Muscle types
- Smooth
- Arteries, hair follicles, uterus, intestines
- Regulated by ANS (involuntary)
- Striated (striped)
- Skeletal
- Voluntary control, mostly connected to tendons and bones
- Cardiac
Muscle types
How skeletal muscles contract
- Motoneuron (ventral horn of spinal cord)
- Neuromuscular junction
- Releases ACh
From spinal cord to muscle
How skeletal muscles contract
- Motor endplate
- Contains nicotinic ACh receptor
- Generates…
- Excitatory endplate potential
- Muscle fibers depolarize
- Depolarization spreads along fibers like an action potential
- Sarcomeres are segments of fibers
- Intramuscular storage sites release Ca++
Motor endplate
How skeletal muscles contract
- Myofibrils (w/in sarcomere)
- Actin & mysosin proteins
- “Molecular gears”
- Bind, move, unbind in presence of Ca++ pllus energy source (ATP)
Anatomy of muscle fibers
Anatomy of motor endplate
Agonist/antagonist muscle pairs
Meat preference?
Muscle fiber types
- Fast twitch/fatiguing
- Type II
- White meat
- Slow twitch/fatiguing
- Type I
- Red meat
Muscles are sensory organs, too!

Two muscle fiber types
Two muscle fiber types
- Intrafusal fibers
- Sense length/tension
- Contain muscle spindles linked to Ia afferents
- ennervated by gamma (\(\gamma\)) motor neurons
- Extrafusal fibers
- Generate force
- ennervated by alpha (\(\alpha\)) motor neurons
Monosynaptic stretch (myotatic) reflex
- Muscle stretched (length increases)
- Muscle spindle in intrafusal fiber activates
- Ia afferent sends signal to spinal cord
- Activates alpha (\(\alpha\)) motor neuron
- Muscle contracts, shortens length
Monosynaptic stetch (myotatic) reflex
- Gamma (\(\gamma\)) motor neuron fires to take up intrafusal fiber slack
https://www.nytimes.com/2020/11/09/sports/emily-harrington-free-climb-yosemite.html
Monosynaptic stretch (myotatic) reflex
Why doesn’t antagonist muscle respond?
Why doesn’t antagonist muscle respond?
- Polysynaptic inhibition of antagonist muscle
- Prevents/dampens tremor
Brain gets fast(est) sensory info from spindles
How the brain controls the muscles
- Pyramidal system
- Pyramidal cells (from Cerebral Cortex Layer 5) in primary motor cortex (M1)
- Corticobulbar (cortex -> brainstem) tract
- Corticospinal (cortex -> spinal cord) tract
- Crossover (decussate) in medulla
- L side of brain ennervates R side of body
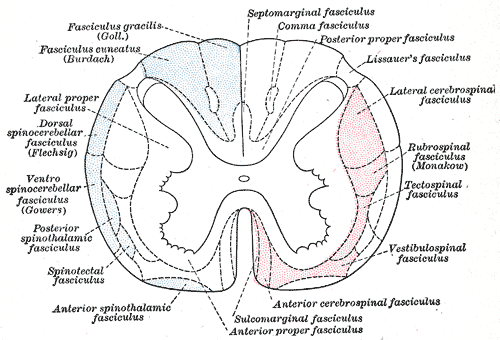
Corticospinal tract
How the brain controls the muscles
- Extrapyramidal system
- Tectospinal tract
- Vestibulospinal tract
- Reticulospinal tract
- Involuntary movements
- Posture, balance, arousal
Extrapyramidal system
This figure shows that the descending motor pathways in red on the right have their own spatial organization depending on where they originate in the brain.
Disorders
- Parkinson’s
- Huntington’s
The Faces of Parkinson’s
Parkinson’s
- Slow, absent movement, resting tremor
- Cognitive deficits, depression
- DA Neurons in substantia nigra degenerate
- Treatments
- DA agonists
- DA agonists linked to impulse control disorders in ~1/7 patients (Ramirez-Zamora, Gee, Boyd, & Biller, 2016)
- Levodopa (L-Dopa), DA precursor
Huntington’s
Huntington’s
- Formerly Huntington’s Chorea
- “Chorea” from Greek for “dance”
- “Dance-like” pattern of involuntary movements
- Cognitive decline
- Genetic + environmental influences
- Disturbance in striatum
- No effective treatment
Huntington’s
Final thoughts
- Control of movement determined by multiple sources
- Cerebral cortex + basal ganglia + cerebellum + spinal circuits
Next time…
- Vision
- Review for Exam 3
References
Borbiro, I., Badheka, D., & Rohacs, T. (2015). Activation of TRPV1 channels inhibits mechanosensitive piezo channel activity by depleting membrane phosphoinositides. Sci. Signal., 8(363), ra15. https://doi.org/10.1126/scisignal.2005667
Melzack, R., & Wall, P. D. (1965). Pain mechanisms: A new theory. Science, 150(3699), 971–979. https://doi.org/10.1126/science.150.3699.971
Papini, M. R., Fuchs, P. N., & Torres, C. (2015). Behavioral neuroscience of psychological pain. Neurosci. Biobehav. Rev., 48, 53–69. https://doi.org/10.1016/j.neubiorev.2014.11.012
Ramirez-Zamora, A., Gee, L., Boyd, J., & Biller, J. (2016). Treatment of impulse control disorders in Parkinson’s disease: Practical considerations and future directions. Expert Review of Neurotherapeutics, 16(4), 389–399. https://doi.org/10.1586/14737175.2016.1158103
Wager, T. D., Atlas, L. Y., Lindquist, M. A., Roy, M., Woo, C.-W., & Kross, E. (2013). An fMRI-based neurologic signature of physical pain. N. Engl. J. Med., 368(15), 1388–1397. https://doi.org/10.1056/NEJMoa1204471