- Somatosensation
- Exteroception via
- Cutaneous receptors + proprioception
- Interoception via
- Widely distributed receptors
- Specific and non-specific
- Exteroception via
2022-04-05 14:25:23
Prelude 3:46
Prelude 2:49
Announcements
- Papers or final blog post due Next Tuesday, April 12
Today’s Topics
- More on somatosensation
- Pain
- Action!
Somatosensation
From skin to brain
- Cutaneous receptors
- Dorsal root ganglion
- Ventral posterior lateral thalamus
- Primary somatosensory cortex (S-I)
- Post-central gyrus of parietal lobe
Dermatomes
Dermatomes
Functional segregation

Functional segregation
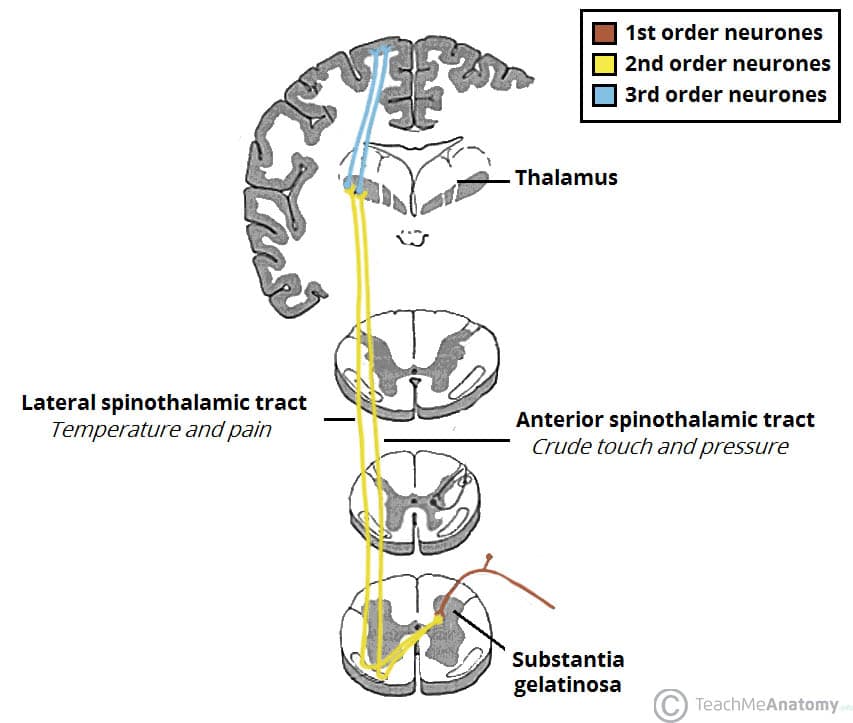
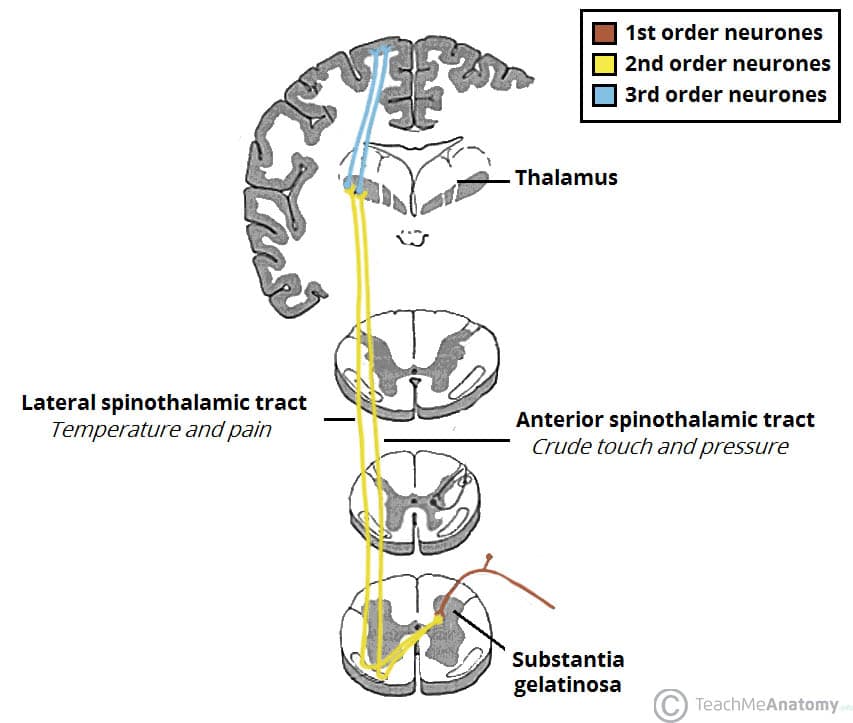
- Separate pathways for different information types
- Dorsal column/medial leminiscal pathway
- Touch, proprioception
- Spinothalamic tract
- Pain, temperature
Somatatopic maps
Non-uniform mapping of skin surface
Non-uniform mapping of skin surface
Columnar organization/functional segregation
Phantom Limbs
What/where
- Perceiving Where
- Somatotopic maps – where on skin
- Kinesthesia – configuration of limbs
- Perceiving What
- Patterns of smoothness, roughness, shape, temperature
Somatosensation in other animals

Pain
The neuroscience of pain
- Nociceptors (Latin nocere to harm or hurt) detect harmful or potentially harmful stimuli of varied types:
- chemical
- mechanical
- thermal
Nociception
- External
- Skin, cornea (eye), mucosa
- Internal
- Muscles, joints, bladder, gut
Different types of nociceptors…
- metabolism (acidic pH, hypoxia, …)
- cell rupture (ATP and glutamate)
- cutaneous parasite penetration (histamine)
- mast cell (white blood cell) activation (serotonin, bradykinin, …)
- immune and hormonal activity (cytokines and somatostatin)
Fast (\(A\delta\)) and slow (\(C\)) transmission to CNS
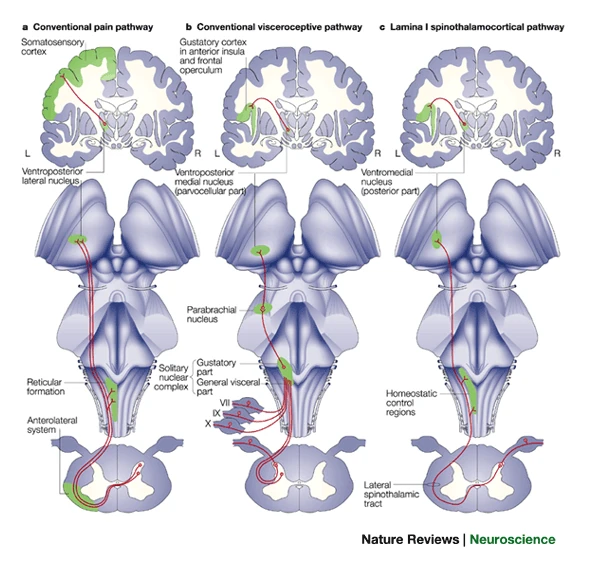
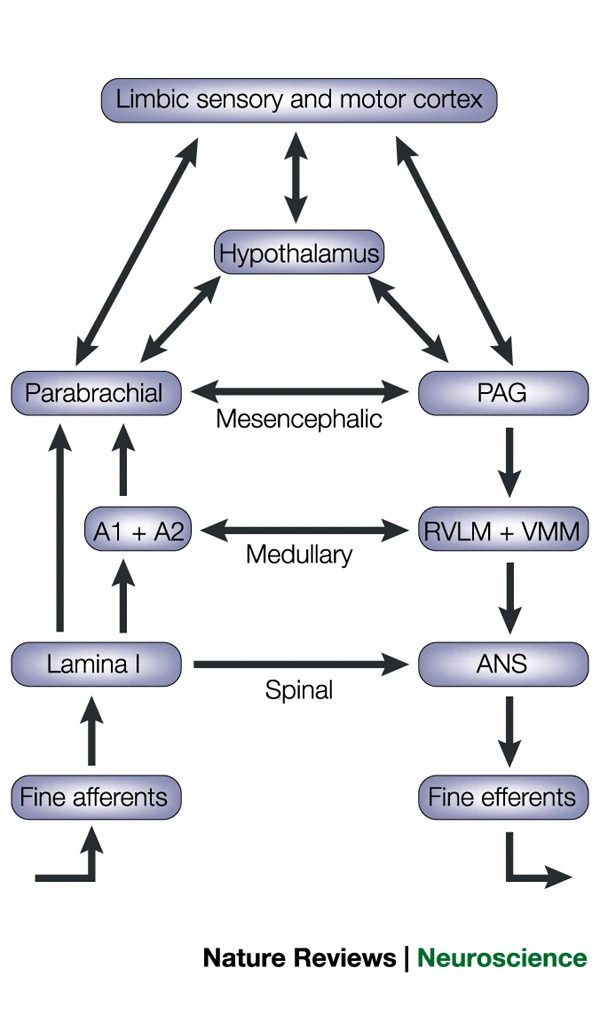
Projection to brain via anterolateral system
Key CNS nodes in network
- Periaqueductal grey (PAG) in midbrain
- Insular cortex (insula)
- Hypothalamus
- Amygdala
Key CNS nodes in network
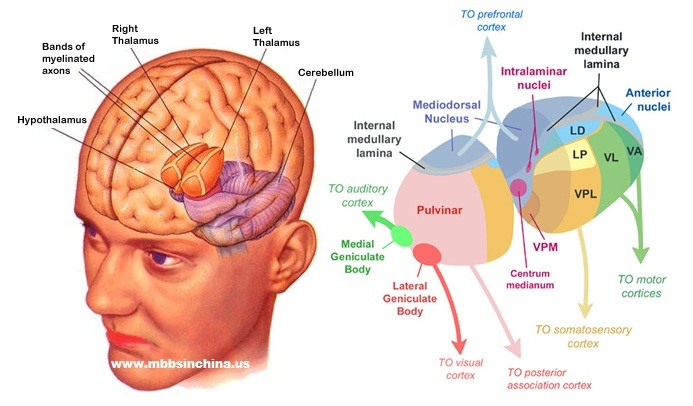
- Thalamus
- Ventroposterior lateral nucleus
- Ventroposterior medial nucleus
- Ventromedial nucleus
Pain in the brain
Pain in the brain
“…we used machine-learning analyses to identify a pattern of fMRI activity across brain regions — a neurologic signature — that was associated with heat-induced pain. The pattern included the thalamus, the posterior and anterior insulae, the secondary somatosensory cortex, the anterior cingulate cortex, the periaqueductal gray matter, and other areas…”
Pain relief
- Prostaglandins
- hormone-like effects, but released in many places
- trigger vasodilation and inflammation
Pain relief
- Paracetymol (acetaminophen)
- Mechanism not fully understood
- inhibits synthesis of prostaglandins via cyclooxygenase (COX) enzyme
- may modulate endocannabinoid system
- Nonsteroidal anti-inflamatory drugs (NSAIDs): aspirin, ibuprofen
- Also inhibit prostaglandins via COX
Pain relief
- Opioids
- Activate endogenous opioid systems
- multiple receptor types (\(\delta\), \(\kappa\), \(\mu\),…)
- peripheral sensory neurons, amygdala, hypothalamus, PAG, spinal cord, cortex, medulla, pons,…
- brainstem opioid neurons provide descending inhibition of nociceptors


Pain relief
- Capsaicin
- Binds to TrpV1/VR1 thermo/nociceptors
- Eventually causes decrease in TrpV1 response
- Alters how peripheral neuron responds to mechanical stimulation
- (Borbiro, Badheka, & Rohacs, 2015)
Pain relief
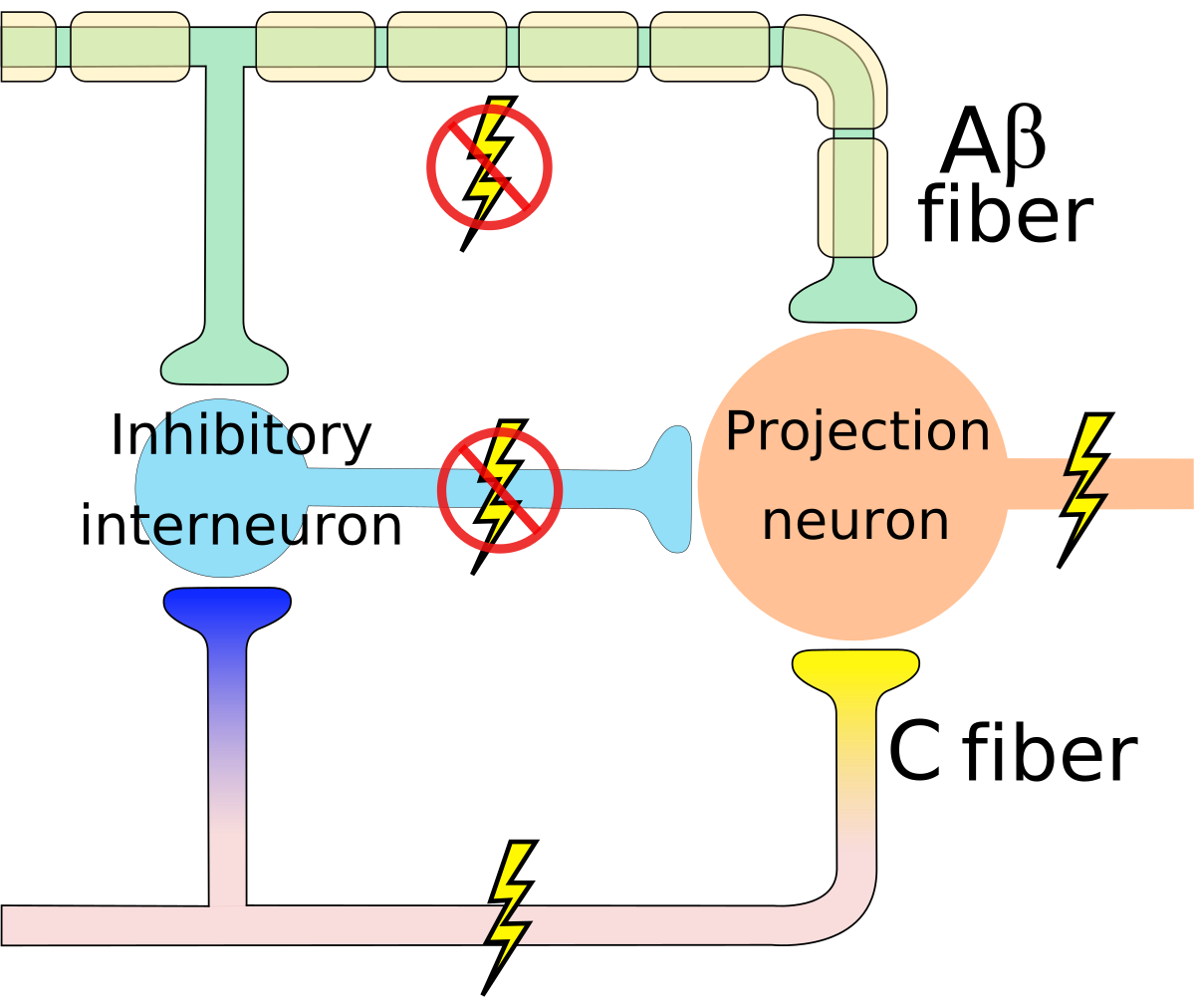
- Why rubbing can help
Gate control theory (Melzack & Wall, 1965)
Gate control theory (Melzack & Wall, 1965)
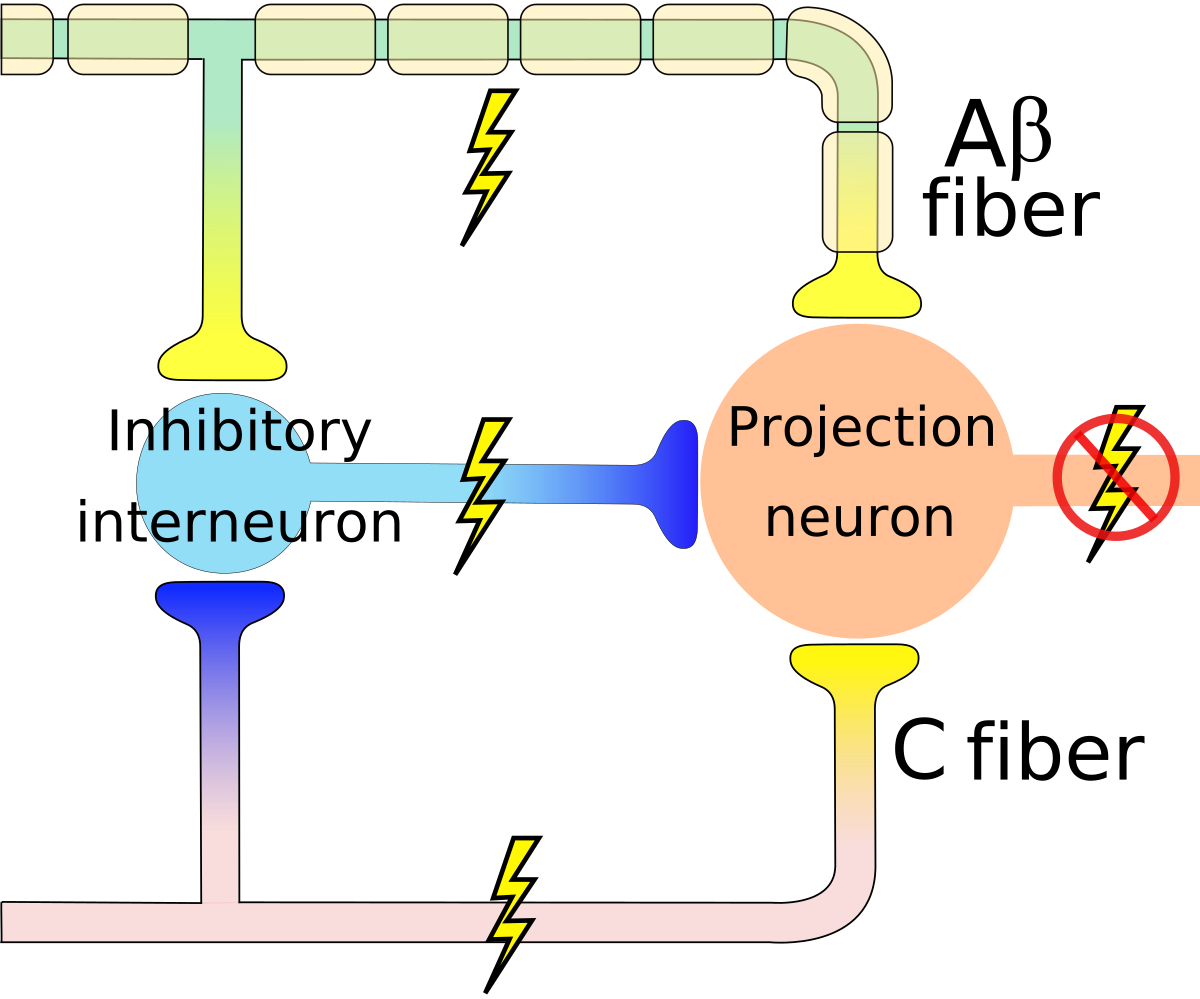
By self - self-made in Inkscape, CC BY-SA 3.0, Link
Psychological & physical components of pain
Main points
Main points
- Pain
- Multiple receptor channels
- Highly interconnected CNS network
- Multiple targets for modulation
Action
The neuroscience of action
- What types of actions are there?
- How are they produced?
- By the muscles
- By the nervous system
Remember
- Nervous system “output” includes
- Movements
- Autonomic responses
- Endocrine responses
Types of actions
- Reflexes
- Simple, highly stereotyped, unlearned, rapid
- vs. Planned or voluntary actions
- Complex, flexible, acquired, slower
- Discrete (reaching) vs. rhythmic (walking)
- Ballistic (no feedback) vs. controlled (feedback)
Multiple, parallel controllers
Key “nodes” in network
- Primary motor cortex (M1)
- Non-primary motor cortex
- Basal ganglia
- Brain stem
- Cerebellum
- Spinal cord
Muscle classes
- Axial
- Trunk, neck, hips
- Proximal
- Shoulder/elbow, pelvis/knee
- Distal
- Hands/fingers, feet/toes
Muscles
Muscle types
- Smooth
- Arteries, hair follicles, uterus, intestines
- Regulated by ANS (involuntary)
- Striated (striped)
- Skeletal
- Voluntary control, mostly connected to tendons and bones
- Cardiac
Muscle types
How skeletal muscles contract
- Motoneuron (ventral horn of spinal cord)
- Neuromuscular junction
- Releases ACh
From spinal cord to muscle
Next time…
- More on action
References
Borbiro, I., Badheka, D., & Rohacs, T. (2015). Activation of TRPV1 channels inhibits mechanosensitive piezo channel activity by depleting membrane phosphoinositides. Sci. Signal., 8(363), ra15. https://doi.org/10.1126/scisignal.2005667
Craig, A. D. (2002). How do you feel? Interoception: The sense of the physiological condition of the body. Nat. Rev. Neurosci., 3(8), 655–666. https://doi.org/10.1038/nrn894
Melzack, R., & Wall, P. D. (1965). Pain mechanisms: A new theory. Science, 150(3699), 971–979. https://doi.org/10.1126/science.150.3699.971
Papini, M. R., Fuchs, P. N., & Torres, C. (2015). Behavioral neuroscience of psychological pain. Neurosci. Biobehav. Rev., 48, 53–69. https://doi.org/10.1016/j.neubiorev.2014.11.012
Wager, T. D., Atlas, L. Y., Lindquist, M. A., Roy, M., Woo, C.-W., & Kross, E. (2013). An fMRI-based neurologic signature of physical pain. N. Engl. J. Med., 368(15), 1388–1397. https://doi.org/10.1056/NEJMoa1204471